Mirtazapine 15mg benefits
Coadministration may result in elevated plasma concentrations of mirtazapine and an increased risk for adverse events, including QT prolongation and TdP. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and lapatinib.
Coadminister with caution and consider ECG and electrolyte monitoring. Lapatinib has been associated with concentration-dependent QT prolongation; ventricular arrhythmias and TdP have been reported in postmarketing experience.
Correct hypokalemia or hypomagnesemia prior to lapatinib administration. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and lenvatinib. Cases of QT prolongation, TdP, ventricular tachycardia, and sudden death have been reported during postmarketing use of mirtazapine, primarily in the setting of mirtazapine overdose or in patients with other risk factors for QT prolongation, including concomitant use of other medications associated with QT prolongation.
QT prolongation was reported during clinical trials of lenvatinib. Moderate There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and leuprolide.
Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and levofloxacin. Levofloxacin has been associated with a risk of QT prolongation and there have been extremely rare reports of TdP during postmarketing use.
Moderate Consistent with the pharmacology of mirtazapine and the drug's side effect profile, additive effects may occur with other CNS-active agents including levomethadyl. Mirtazapine should be administered with caution with such agents because the CNS effects on cognitive performance and motor skills can be additive.
Major Because of the potential risk and severity of serotonin syndrome, caution should be observed when coadministering drugs that have serotonergic properties such as mirtazapine and levomilnacipran. Moderate Concomitant use of levorphanol with other CNS depressants such as mirtazapine can potentiate the effects of levorphanol on respiration, blood pressure, and alertness.
Severe hypotension, respiratory depression, profound sedation, or coma may occur. Prior to concurrent use of levorphanol in patients taking a CNS depressant, assess the level of tolerance to CNS depression that has developed, the duration of use, and the patient's overall response to treatment.
When concomitant treatment with levorphanol with another CNS depressant is necessary, reduce the dose of 1 or both drugs. Severe Treatment initiation with heterocyclic antidepressants e. If urgent psychiatric treatment is required, interventions other than these antidepressants e.
Conversely, in patients receiving these antidepressants and requiring urgent treatment with linezolid, the antidepressant should be discontinued immediately and linezolid therapy initiated only if acceptable alternatives are not available and the potential benefits of linezolid outweigh the risks.
The patient should be monitored for serotonin syndrome for 2 weeks or until 24 hours after the last dose of linezolid, whichever comes first. The antidepressant may be re-initiated 24 hours after the last dose of linezolid Lisdexamfetamine: Moderate Because of the potential risk and severity of serotonin syndrome, caution should be observed when administering mirtazapine with other drugs that have serotonergic properties such as lisdexamfetamine.
Patients receiving mirtazapine and lisdexamfetamine should be monitored for the emergence of serotonin syndrome. Lithium and mirtazapine have been associated with QT prolongation.
Lithium has been reported to increase 5-hydroxytryptamine metabolites in the cerebrospinal fluid and may interact pharmacodynamically with serotonergic agents such as mirtazapine to cause serotonin syndrome.
Moderate There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and loperamide. At high doses, loperamide has been associated with serious cardiac toxicities, including syncope, ventricular tachycardia, QT prolongation, TdP, and cardiac arrest. Severe Lopinavir; ritonavir is associated with QT prolongation. Coadministration of lopinavir; ritonavir with other drugs that prolong the QT interval, such as mirtazapine, may result in additive QT prolongation.
In addition, ritonavir is a potent CYP3A4 inhibitor and coadministration with other drugs metabolized by CYP3A4 where an increase in serum concentrations would lead to serious adverse effects is contraindicated. Moderate Lumacaftor; ivacaftor may reduce the efficacy of mirtazapine by decreasing its systemic exposure; if used together, it may be necessary to increase the mirtazapine dose to achieve clinical efficacy.
If lumacaftor; ivacaftor is subsequently discontinued, consider mirtazapine dosage reduction. Mirtazapine is a substrate of CYP3A. Lumacaftor is a strong CYP3A inducer. Minor Because of the CNS-depressant effects of magnesium sulfate, additive central-depressant effects can occur following concurrent administration with CNS depressants such as heterocyclic antidepressants.
Caution should be exercised when using these agents concurrently. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and maprotiline.
In addition, these medications may be duplicate treatment for some conditions. Maprotiline has been reported to prolong the QT interval, particularly in overdose or with higher-dose prescription therapy elevated serum concentrations. Cases of long QT syndrome and TdP tachycardia have been described with maprotiline use, but rarely occur when the drug is used alone in commonly prescribed doses and in the absence of other known risk factors for QT prolongation.
Limited data are available regarding the safety of maprotiline in combination with other QT-prolonging drugs. Moderate Consistent with the CNS depressant effects of mirtazapine, additive effects may occur with other CNS depressants such as meclizine. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and mefloquine. There is evidence that the use of halofantrine after mefloquine causes a significant lengthening of the QTc interval.
Mefloquine alone has not been reported to cause QT prolongation. However, due to the lack of clinical data, mefloquine should be used with caution in patients receiving drugs that prolong the QT interval. A dose reduction of one or both drugs may be warranted to avoid additive effects.
Due to the possibility of additive effects on the QT interval, caution is advisable during concurrent use of mesoridazine and mirtazapine. Mesoridazine, a phenothiazine, is associated with an established risk of QT prolongation and torsade de pointes TdP.
Major Coadministration of methadone with drugs known to prolong the QT interval, such as mirtazapine, should be done with extreme caution and a careful assessment of risks versus benefits. Most cases involve patients being treated for pain with large, multiple daily doses of methadone, although there are reports in patients receiving doses commonly used for maintenance treatment of opioid addiction.
In addition, concomitant use of methadone and other CNS depressants such as mirtazapine can lead to additive respiratory depression, hypotension, profound sedation, or coma. Prior to using methadone in patients taking a CNS depressant, assess the level of tolerance to CNS depression, the duration of use, and the patient's overall response to treatment.
Assess alcohol or illicit drug use. Reduced dosages of methadone should be used with other CNS depressants. In opioid-naive adults, use an initial methadone dose of 2. Also consider using a lower dose of the CNS depressant. Moderate Because of the potential risk and severity of serotonin syndrome, caution should be observed when administering mirtazapine with other drugs that have serotonergic properties such as methamphetamine.
Patients receiving mirtazapine and methamphetamine should be monitored for the emergence of serotonin syndrome. Moderate Because of the potential risk and severity of serotonin syndrome, caution should be observed when coadministering drugs that have serotonergic properties such as methylphenidate and mirtazapine.
Other drugs that may also cause drowsiness, such as mirtazapine, should be used with caution. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and midostaurin. QT prolongation was reported in patients who received midostaurin in clinical trials.
Consider obtaining electrocardiograms to monitor the QT interval if it is used with other drugs that prolong the QT interval. Moderate There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and mifepristone RU Mifepristone has been associated with dose-dependent prolongation of the QT interval.
To minimize the risk of QT prolongation, the lowest effective dose of mifepristone should always be used. Major Because of the potential risk and severity of serotonin syndrome, caution should be observed when coadministering drugs that have serotonergic properties such as mirtazapine and milnacipran. Minor Injectable minocycline contains magnesium sulfate heptahydrate.
Because of the CNS-depressant effects of magnesium sulfate, additive central-depressant effects can occur following concurrent administration with CNS depressants such as heterocyclic antidepressants i. Exposure of drugs partially metabolized by CYP2D6 such as mirtazapine may be increased when co-administered with mirabegron. Appropriate monitoring and dose adjustment may be necessary.
Major Use caution if mitotane and mirtazapine are used concomitantly, and monitor for decreased efficacy of mirtazapine and a possible change in dosage requirements.
Mitotane is a strong CYP3A4 inducer and mirtazapine is a CYP3A4 substrate; coadministration may result in decreased plasma concentrations of mirtazapine.
Moderate Molindone may cause central nervous system CNS depression thereby having additive effects with other drugs that can cause CNS depression such as mirtazapine. Caution is advisable during concurrent use. Major Concomitant use of morphine with other CNS depressants can potentiate the effects of morphine on respiration, blood pressure, and alertness; examples of other CNS depressants include mirtazapine.
Prior to concurrent use of morphine in patients taking a CNS depressant, assess the level of tolerance to CNS depression that has developed, the duration of use, and the patient's overall response to treatment. In addition, because of the potential risk and severity of serotonin syndrome, caution and careful monitoring are recommended when coadministering drugs with serotonergic properties such as morphine and mirtazapine.
Morphine and mirtazapine should be discontinued if serotonin syndrome occurs and supportive symptomatic treatment should be initiated. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and moxifloxacin. Although extremely rare, TdP has been reported during postmarketing surveillance of moxifloxacin. These reports generally involved patients with concurrent medical conditions or concomitant medications that may have been contributory.
Moderate Nabilone or other CNS depressants should be combined cautiously with heterocyclic antidepressants because they could cause additive depressant effects and possible respiratory depression or hypotension. Moderate Concomitant use of nalbuphine with other CNS depressants, such as mirtazapine, can potentiate the effects of nalbuphine on respiratory depression, CNS depression, and sedation. Major Because of the potential risk and severity of serotonin syndrome, caution should be observed when administering mirtazapine with other drugs that have serotonergic properties such as nefazodone.
Additive sedative effects are also possible. Moderate Concurrent administration of mirtazapine and nelfinavir may result in elevated mirtazapine plasma concentrations.
Major Because of the potential risk and severity of serotonin syndrome, use caution when administering palonosetron with other drugs that have serotonergic properties such as mirtazapine. If serotonin syndrome is suspected, discontinue palonosetron and concurrent serotonergic agents and initiate appropriate medical treatment.
Serotonin syndrome is characterized by rapid development of hyperthermia, hypertension, myoclonus, rigidity, autonomic instability, mental status changes e. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and nilotinib.
According to the manufacturer, nilotinib therapy should be interrupted if treatment with another drug that prolongs the QT interval is required.
If interruption of treatment with nilotinib is not possible, closely monitor for evidence of QT prolongation during concurrent use. Minor Nitroglycerin can cause hypotension. This action may be additive with other agents that can cause hypotension such as antidepressants.
Patients should be monitored more closely for hypotension if nitroglycerin is used concurrently with antidepressants. Moderate There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and norfloxacin. Quinolones have been associated with a risk of QT prolongation and TdP. Although extremely rare, TdP has been reported during postmarketing surveillance of norfloxacin.
Moderate There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and octreotide. Arrhythmias, sinus bradycardia, and conduction disturbances have occurred during octreotide therapy. Since bradycardia is a risk factor for development of TdP, the potential occurrence of bradycardia during octreotide administration could theoretically increase the risk of TdP in patients receiving drugs that prolong the QT interval.
Until further data are available, it is suggested to use octreotide cautiously in patients receiving drugs which prolong the QT interval. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and ofloxacin. Although extremely rare, TdP has been reported during postmarketing surveillance of ofloxacin. Major Concomitant use of mirtazapine and ondansetron may increase the risk of serotonin syndrome, QT prolongation, and torsade de pointes.
If ondansetron and another drug that prolongs the QT interval must be coadministered, ECG monitoring is recommended. Ondansetron has been associated with a dose-related increase in the QT interval and postmarketing reports of TdP. In addition, both mirtazapine and ondansetron have central serotonin-enhancing effects; therefore, serotonin syndrome is possible.
Major Monitor electrolytes and ECGs for QT prolongation if coadministration of mirtazapine with osimertinib is necessary; an interruption of osimertinib therapy and dose reduction may be necessary if QT prolongation occurs.
Both drugs have been associated with dose-dependent prolongation of the QT interval. Torsade de pointes TdP has been reported in postmarketing experience with mirtazapine, primarily in overdose or in patients with other risk factors for QT prolongation.
Major Monitor electrolytes and ECGs for QT prolongation if coadministration of mirtazapine with oxaliplatin is necessary; correct electrolyte abnormalities prior to administration of oxaliplatin.
QT prolongation and ventricular arrhythmias including fatal TdP have also been reported with oxaliplatin use in postmarketing experience.
Hypotension, profound sedation, coma, respiratory depression, or death may occur; examples of other CNS depressants include mirtazapine. Prior to concurrent use of oxymorphone in patients taking a CNS depressant, assess the level of tolerance to CNS depression that has developed, the duration of use, and the patient's overall response to treatment.
If the extended-release oxymorphone tablets are used concurrently with a CNS depressant, it is recommended to use an initial dosage of 5 mg PO every 12 hours. Monitor for sedation or respiratory depression. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and paliperidone. According to the manufacturer of paliperidone, use of the drug should be avoided with agents known to prolong the QT interval since paliperidone also has this effect.
However, if concurrent use is necessary and the patient has risk factors for cardiac disease or arrhythmias, close monitoring is essential. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and panobinostat.
QT prolongation has been reported with panobinostat and concurrent use with other agents that prolong the QT interval is not recommended. Major Because of the potential risk and severity of serotonin syndrome or neuroleptic malignant syndrome-like reactions, caution should be observed when administering paroxetine with other drugs that have serotonergic properties such as mirtazapine.
Increased mirtazapine serum concentrations may occur following the addition of a potent CYP2D6 inhibitor such as paroxetine to a stable mirtazapine regimen. Patients receiving this combination should be monitored for the emergence of serotonin syndrome, neuroleptic malignant syndrome-like reactions, or other adverse effects. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and pasireotide. QT prolongation has occurred with pasireotide at therapeutic and supra-therapeutic doses.
Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and pazopanib. Coadministration of pazopanib and other drugs that prolong the QT interval is not advised. If pazopanib and mirtazapine must be coadministered, closely monitor for QT prolongation. Moderate Monitor for adverse effects associated with increased exposure to mirtazapine if peginterferon alfa-2b is coadministered.
Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and pentamidine. Systemic pentamidine has been associated with QT prolongation. The combination of perampanel particularly at high doses with ethanol has led to decreased mental alertness and ability to perform complex tasks such as driving , as well as increased levels of anger, confusion, and depression; similar reactions should be expected with concomitant use of other CNS depressants, such as mirtazapine.
Due to the possibility of additive effects on the QT interval, caution is advisable during concurrent use of mirtazapine and perphenazine. Perphenazine is associated with a possible risk for QT prolongation, particularly in overdose settings. Theoretically, perphenazine may increase the risk of QT prolongation if coadministered with other drugs that have a risk of QT prolongation. Because both mirtazapine and perphenazine have CNS depressant properties, patients should be advised to avoid engaging in activities requiring mental alertness until they are aware of the effects of the combination.
Major Because of the potential risk and severity of serotonin syndrome, caution should be observed during co-administration of mirtazapine with other drugs that have serotonergic properties. As a drug related to the amphetamines, phentermine has the potential to cause serotonin syndrome when combined with serotonergic agents. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and pimavanserin. Pimavanserin may cause QT prolongation and should generally be avoided in patients receiving other medications known to prolong the QT interval.
Severe Because of the potential for torsade de pointes TdP , concurrent use of pimozide and mirtazapine is contraindicated. Pimozide is associated with a well established risk of QT prolongation and TdP. Posaconazole has been associated with QT prolongation and torsade de pointes TdP.
Cases of QT prolongation, TdP, ventricular tachycardia, and sudden death have been reported during postmarketing use of mirtazapine, primarily following overdose or in patients with other risk factors for QT prolongation.
Moderate Some medicines used for treatment of Parkinson's disease, like pramipexole, could potentially cause additive drowsiness when coadministered with mirtazapine. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and primaquine. Primaquine has the potential for QT interval prolongation. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and procainamide.
Procainamide is associated with a well-established risk of QT prolongation and TdP. Severe Use of mirtazapine concurrently with drugs that exhibit MAO-inhibition, such as procarbazine, is contraindicated. If combined, there is a possibility of developing serious reactions such as hyperpyrexia, hypertension, or seizures.
An interval of 14 days is recommended between cessation of MAOI therapy and initiation of mirtazapine therapy and vice versa. Due to the possibility of additive effects on the QT interval, caution is advisable during concurrent use of mirtazapine and prochlorperazine. Prochlorperazine is associated with a possible risk for QT prolongation, particularly in overdose settings. Theoretically, prochlorperazine may increase the risk of QT prolongation if coadministered with other drugs that have a risk of QT prolongation.
Because both mirtazapine and prochlorperazine have CNS depressant properties, patients should be advised to avoid engaging in activities requiring mental alertness until they are aware of the effects of the combination. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and propafenone.
Moderate Consistent with the pharmacology of mirtazapine and the CNS depression that may occur, additive effects may occur with other CNS depressants, including propofol.
Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent use of mirtazapine and quetiapine. The manufacturer of quetiapine recommends avoiding combined use of quetiapine with drugs known to increase the QT interval.
Limited data, including some case reports, suggest that quetiapine may be associated with a significant prolongation of the QTc interval in rare instances. Because both mirtazapine and quetiapine can cause somnolence, monitoring for additive CNS depressant effects is recommended. The next night I managed to sleep a total of 5. I think one of the key factors for getting through this is that I have lowered my expectations on sleep. I used to get knocked out for 8 hours or more on the Mirtazapine so used to think that this was normal.
Good luck to everyone coming off Mirtazapine. You will get through it eventually once your body and brain have learnt to cope on their own again. It WILL eventually get better! Reply Link Julia November 14, , 4: The turning point for me was believing that I could sleep on my own and when I accepted the fact that I would have some bad nights sleep and stopped fighting the anxiety.
I also changed my outlook on everything so instead of feeling victimised by the withdrawal symptoms I got angry at them and refused to let them stop me from living my life.
I hope I managed to give some hope to anyone whose considering coming off this medication or is suffering from withdrawal. Stick with it and get help — you can do this! Reply Link Liz August 30, , 7: I appreciate seeing that you went off, and then back on, but were able to come off. Reply Link Anne November 3, , 1: I have been going for EMDR therapy and after 20 sessions — three months ago — I felt I had dealt with a childhood trauma which was causing the severe depression. In April I stopped taking Diazepam and then a beta blocker — all successfully!
They were both causing side effects. Effects that only developed this year. A month ago I started tapering off the Mirtazapine as I started with a new side effect! I also believe my body is producing the necessary chemicals naturally. As it should be. So far no withdrawal symptoms. This is my experience and in no way do I think others will be like me. All I would say is that at the time I needed the medication to prop me up so I could do the therapy.
I wish you all well. And I am sooo glad I feel joy and peace in my life now. But three years on I feel repaired.
Reply Link Robb November 5, , 4: It has turned out to be my guide the last couple of weeks. Information about quitting antidepressants is so minimal! After having a very bad experience with strange hallucinations caused by citalopram, I tried mirt as a kind of last resort. All my anxiety problems intensed again hallucinations and strange new phobias started to develop. But the docs said keep going these meds take time to work!
So I decided to quit and face my problems myself without antidepressants. I used 15 mg for 4. First 2 weeks were living hell. This week things are getting better but still not good enough. Any of you had similar experiences? I am hoping to see some light at the end of the tunnel the coming days.
R Reply Link Robb November 17, , 3: It has now been a month 33 days since my last 3. Finally I am noticing that the anxiety is starting to lift, also I am noticing that some of my phobias knives, driving are clearing out. I am using magnesium and fish oil supplements as well. Alas for me I seem to have developed a kind of OCD during my treatment with mirt.
I took my last mirt 5 months ago. I thought all was going well until 4 weeks ago when drastic weight loss kicked in. The more I ate, the more I seemed to lose. My heart rate was going nuts and that was bringing back the old anxiety. I had a pain in my neck and found a lump. After scanning and blood tests, nodules were discovered on my thyroid.
I have had routine thyroid testing my whole life and never had a problem until coming off the mirtazpine. I am wondering now if others like David who have lost huge amounts of weight have had their thyroid tested. My doctors first reaction was to put me back on mirt to bring my heart rate down blaming this on anxiety. David if you read this, I would be interested to know your thoughts.
Reply Link Mel November 7, , I tried to taper off about 4 months ago but found the panic attacks and incessant crying too much to handle. I have now been off Remeron cold turkey for 3weeks. I had food poisoning and was unable to take it for 2 days… then decided the withdrawal symptoms of remeron were similar to food poisoning and that now was the perfect time to try again.
I came across this site today because my main search symptom was itchiness. It now takes me about an hour to fall asleep on the drug, less than a minute I wake up about 4 times during the night startled from vivid and bizarre dreams. I have been trying imagery rehearsal therapy for my sleep issues, meditate daily and practice CBT to calm the oncoming panic attacks only 2 in the last 3 weeks. I am very much trying to stay controlled and relax. I have had one outburst of extreme anger for no apparent reason , at which point I put myself to bed for a couple of hours to recollect.
I know it takes a lot of courage to decide to come off a drug you feel so dependent on and it is very scary to trust in yourself that you can manage your sober mind. Thank you for this site! Reply Link David November 7, , 7: I had said that I would never take another mirt.
Within 24 hours I felt like a new man in every respect, and that was after 8 months off of it in hell. That was a week ago, and I have gained over 10 pounds of my weight back.
If you have a high heart rate and thyroid trouble, those need to be addressed. This is my situation as of the last 8 days, before that I felt like hell, had no appetite, and no energy. I may have to go to the 7. That was the second attempt for me. I hope that this has been helpful.
I would definitely get that thyroid situation taken care of. I know a lady friend who got parathyroid tumor and had to have surgery while coming off mirtazapine.
You can contact her on Facebook, and I will give you her contact name if you e-mail me at dlbx2[AT]outlook. David Reply Link Rachel November 8, , 1: I am hungry all the time.
I have no energy. I constantly think about food… then I feel bloated and fat. My clothes are getting tight! Tired of feeling numb and fuzzy in the head as well. Reply Link Gil Grant November 13, , Simply dropped them and have slept better ever since. Withdrawal effects; never felt better! Reply Link jan November 22, , 9: Just got too sick and down to They put me at 7. Going to new doc on Dec 2 will see what comes of that. I do know now that all of my problems are anxiety that the mirtazapine was taking care of.
Wishing now I had never gone off it. Just opened a can of worms and now having a heck of a time getting back to where I was.
What the heck is that? Will see how my appointment goes. Reply Link wayne bell November 23, , 4: I want to get the word out how hard it is to get off this drug. I am into my 3rd month of being off of Remeron. I am still suffering from certain withdrawal symptoms. The worst is the continuing nausea every morning.
I have yet to throw up once, but it is worse I think to feel the nausea and NOT throw up. The only solution I have gotten for this so far is when I get the nausea feeling after waking up I immediately take a dissolving pill called Ondansetron ODT 8mg. The brand name for it is Zofran. CVS is expensive so try another pharmacy. Hopefully this helps anyone with this constant everyday nausea feeling.
I also have problems with schizophrenia at bedtime. The never ending cough and drainage is unimaginable. I pray for quick recovery to get my life back to normal. Reply Link Pam November 24, , 1: I had been on 7. I cut back to 3. I thought hey, this is not bad! So, I then cut back to 0 in October , and started noticing sneezing and a runny nose. I did not make the connection to Mirtazapine, I thought it was allergies.
Then, by late October, I started getting debilitating headaches — sometimes on one side of my head, sometimes the back of my head so that I have to use two pillows at night to sleep. I thought it was hormone related — again, I did not make any connection to Mirtazapine. During this time, I had a hard time sleeping throughout the night — that is the biggest reason I would not give up mirtazapine in recent years. When I went off of the drug, I would wake up several times during the night, maybe stay awake for an hour, fall back asleep.
So, I maybe got hours of sleep per night, sometimes more but it did not seem like the quality of my sleep was good.
Anyway, after suffering through headaches and generally just not feeling good on most days for over a month, I went back on to 3. Part of the impetus was because on Nov 6, I took a 4-hour certification exam for my profession, and although I passed, the headaches bothered me during the exam to the extent that I was worried that I might have to take a break, lose time and potentially not finish and then flunk the exam.
Definitely by 2 days later, I was pretty much back to normal while on the 3. I thought it was because I was sleeping better and the pressure of the exam was over, I did not attribute it to the drug.
So, I decided to go off the drug again on Nov I did OK for about 3 to 4 days but then, the headaches and flu like symptoms kicked in. This time, I had no particular pressure to point the finger at and even had a day off. I had a hard time finishing out the day at work 4 days after going to 0 and had to lay down.
I could not eat any dinner and thought I was going to be ill. I went back on to 3. So, my plan now is to stay on the 3. I do think that being on the drug for almost 2 decades must have done something to my brain chemistry such that even a small dose makes a difference and I need to taper off to 0 very carefully.
Reply Link Christina November 29, , 2: So all that to say, we split the dose in half 7. Reply Link Gayle December 1, , I was having all the side effects with trips to the emergency room feeling like I was dying.
ER doctors could never find anything wrong. Anyone wanting to get off of this antidepressant should try The Road Back protocol. It it truly helpful…lessens withdrawal symptoms so one can function and sleep at night. Hope this helps someone… Reply Link jan December 3, , 2: She says the symptoms I am experiencing are anxiety and not withdrawal. I finally have to agree. When I withdraw mirtazapine the anxiety kicks in and that stuff can mess up your whole body top to bottom.
This doctor has me on 7. I am going to do my best to do this. I got down to 84 and look awful. Have stopped losing and about 86 lbs now. It took a year to lose that much so I expect it to take awhile to come back. Just want my clear head not dizzy anymore. The dizzy is hard to deal with. Also, this doctor said a person my age 78 should not be taking ativan. I suppose for fear of falling. Wish I could find a more experienced doctor but I live 20 miles from everywhere. Glad you are feeling better David.
Not sure that I will be back into this site. Just want to think positive thoughts and try to feel better and get on with my life. I have taken 15mg of the drug above for 8 years. Over the last 6 months I have reduced that to half 7. Then half every other night gradually trying to get off them. I also have a flu-like cold at the minute. I have started a new course of antidepressants today and have been taking rescue remedy to calm down.
Thanks for the advice. Reply Link Miray December 14, , I am going between 7. Every time I succeed to sleep one night with 3. Can anyone advise any herbal or other additive to get rid of these withdrawal symptoms?
Reply Link Judy December 19, , 8: The lower you get, the more careful you need to be with reductions. It also helps to gather a lot of tools for dealing with insomnia..
Many supplements are often a problem as the nervous system is more sensitized…some people find epsom salts baths helpful, or taking magnesium, or a low dose of melatonin. But the reality is, there will be some degree of sleeplessness during withdrawal.
Careful and slow tapering can help minimize it though. There are lots of resources on the web for meditation or practices mentioned above. It literally saved my life. Check out Lee Holden…he has a couple of free videos posted on youtube. It might be best to wait awhile, for things to stabilize, before weighing and reducing more gradually. Reply Link claudie December 17, , 1: I am wondering if I will ever feel like I did before this drug?
My nerves are not good at all and an emotional rollercoaster. I will never take this drug again and it has made my life hell since coming off it.
I am frustrated and sick of being sick…blessings to all who are going through withdrawals and the hell it causes. The buzzing I still get in my head and dizziness is overwhelming, and I have become a recluse, because being around noise, or any loud levels of laughter, etc. I just want ME back. Reply Link Asha December 19, , 8: I only gained 15 kg but my weight was only 50kg when I started. Reply Link Chris December 21, , The swap over to mirtazapine was terrible for about 3 weeks, but after the usual backward and forward to my doctor, I eventually ended up on 30mg of mirtazapine.
At this time I slept well and mostly all day as well, was becoming less the person I use to be, slow thinking cabbage-head with muscle spikes, restless legs, sore feet and agitated, flu-like symptoms, my dose was then returned to 15mg. By accident my pharmacy gave me the orally dispersible tablets which actually reduced the restless side effect so I asked for these each time I re prescribed.
Temper was like a tickling time bomb and little care for my life and anyone else and 20 pounds heavier. This forum helped me reduce my dose, a little too fast at first… as I suffered panic attacks so I leveled my dose and reduced again maybe 3 weeks later.
I still have side effects 16 weeks after my last dose, weeks off I had suicide ideation. I have seen a private therapist for 6 months and have a very supportive family around me.
The drug alters your mental state which takes as long as it takes to return back to normal, unfortunately this makes you feel like your going back where you started. Reply Link David December 23, , I tapered down to 30 for 1 month then 30 every second day for 1 month then stopped altogether as I said approx 2 months ago.
The lack of sleep and itchiness were the biggest issues. The itchiness stopped after approx 2 weeks. My sleep is also improving heaps. I have also lost weight.
I am also trying to stay more active to combat any negative feelings which does help. I was on antidepressants for approx 5 years with last 2 on this stuff. They did help and I would assess as good and bad. I am looking forward and not back.
I just read a lot of comments regarding how hard it has been and I truly feel for these people. I think timing is everything. My life is as stable as it can be so this is why I chose now. I tried once before when life was very stressful and that was a big mistake. It can be done and you will be fine.
Also be bold and talk to family and friends about how you are feeling. It does make it easier sharing the problem. I wish you all every success. Reply Link Eva December 25, , 9: I been on mirtazapine 7. It was working for 1 month… but I gain some weight and was sleeping very well. Then I felt I was getting more brain zaps and my mood started to change. Decided to stop and went down 3. Was not able to sleep or eat at all. The brain zap is the worst. So scared to stop this, but I have to.
Reply Link Alyssa December 26, , I started them due to some anxiety and insomnia. I want to note that I am not depressed, or do not have an anxiety disorder.
My anxiety was caused by my insomnia. Since going on, my sleep improved wonders. Now, its been 2 months and I have decided to taper off. Only problem is now I am experiencing recurring insomnia. I went down to 7. Please give any advice or indications as to how long this will last! Any tips on how to cope in the meantime would be appreciated. Reply Link Chris December 28, , If you have been on 15mg for 2 months they will have made an impact on you. I broke tablets up, say a 15 mg in half plus say a quarter to make 10mg, did this for a few weeks and reduced again but my sleep pattern was the first thing they hit.
Halving the dose from 15mg to 7. When first diagnosed with clinical depression and anxiety my GP prescribed me Lexapro 10mg to take one every morning and also diazepam 2mg twice a day. My GP had changed my medication to avanza.
I was taking 15mg every night for about 11 days. I had seen my GP 5 days ago explaining to him the symptoms I was having. Every night I would dream of such bad things and I would wake up cause my heart was racing like crazy.
This is no exaggeration I put on 7 kilos in 11 days. Please bear in mind not everyone will put on weight whilst taking this medication. I was also becoming more angry and everyone I know is getting on my nerves. I feel like I have lost myself. My GP told me to take it for another week. So that night I took it, worst heart racing experience I have ever had, my heart was racing that fast it woke me up I was out of breath!!!
I honestly thought I was having a heart attack. So after that night have not taken it since which has been 5 nights now. Although I am still having bad dreams and my heart is racing like mad. Has anyone experienced the crazy heart racing?? I hope whoever is starting or taking this medication will not experience what I have. Reply Link Alison January 3, , 7: Pharmacokinetic studies revealed a decreased clearance in the elderly.
Information for Patients Read the Medication Guide that comes with you or your family member's antidepressant medicine. This Medication Guide is only about the risk of suicidal thoughts and actions with antidepressant medicines.
Talk to your, or your family member's healthcare provider about: Antidepressant medicines may increase suicidal thoughts or actions in some children, teenagers, and young adults within the first few months of treatment. Depression and other serious mental illnesses are the most important causes of suicidal thoughts and actions. Some people may have a particularly high risk of having suicidal thoughts or actions.
These include people who have or have a family history of bipolar illness also called manic-depressive illness or suicidal thoughts or actions. How can I watch for and try to prevent suicidal thoughts and actions in myself or a family member?
Pay close attention to any changes, especially sudden changes, in mood, behaviors, thoughts, or feelings. This is very important when an antidepressant medicine is started or when the dose is changed. Call the healthcare provider right away to report new or sudden changes in mood, behavior, thoughts, or feelings. Keep all follow-up visits with the healthcare provider as scheduled. Call the healthcare provider between visits as needed, especially if you have concerns about symptoms.
Call a healthcare provider right away if you or your family member has any of the following symptoms, especially if they are new, worse, or worry you: In patients who develop these symptoms, increasing the dose may be detrimental.
Hyponatremia Hyponatremia has been reported very rarely with the use of mirtazapine. Caution should be exercised in patients at risk, such as elderly patients or patients concomitantly treated with medications known to cause hyponatremia. In these studies, somnolence resulted in discontinuation for It is unclear whether or not tolerance develops to the somnolent effects of mirtazapine. It is unclear whether or not tolerance develops to the dizziness observed in association with the use of mirtazapine.
Most of these patients with ALT increases did not develop signs or symptoms associated with compromised liver function. While some patients were discontinued for the ALT increases, in other cases, the enzyme levels returned to normal despite continued mirtazapine treatment. Seizure In premarketing clinical trials, only 1 seizure was reported among the US and non-US patients treated with mirtazapine.
However, no controlled studies have been carried out in patients with a history of seizures. Therefore, care should be exercised when mirtazapine is used in these patients. Use in Patients with Concomitant Illness Clinical experience with Mirtazapine Orally Disintegrating Tablets in patients with concomitant systemic illness is limited. Accordingly, care is advisable in prescribing mirtazapine for patients with diseases or conditions that affect metabolism or hemodynamic responses.
Mirtazapine Orally Disintegrating Tablets have not been systematically evaluated or used to any appreciable extent in patients with a recent history of myocardial infarction or other significant heart disease. Mirtazapine was associated with significant orthostatic hypotension in early clinical pharmacology trials with normal volunteers.
Orthostatic hypotension was infrequently observed in clinical trials with depressed patients. Mirtazapine Orally Disintegrating Tablets should be used with caution in patients with known cardiovascular or cerebrovascular disease that could be exacerbated by hypotension history of myocardial infarction, angina, or ischemic stroke and conditions that would predispose patients to hypotension dehydration, hypovolemia, and treatment with antihypertensive medication.
Information for Patients Prescribers or other health professionals should inform patients, their families, and their caregivers about the benefits and risks associated with treatment with Mirtazapine Orally Disintegrating Tablets and should counsel them in its appropriate use.
The prescriber or health professional should instruct patients, their families, and their caregivers to read the Medication Guide and should assist them in understanding its contents.
Side effects of baclofen and tips for managing them
 Moderate Mirtazapine with the pharmacology of mirtazapine and the CNS depression that may occur, benefit effects may occur with other CNS depressants, including etomidate. The first night I slept for about 16 hours! Pay close attention to any changes, especially sudden changes, in mood, behaviors, mirtazapine 15mg benefits, thoughts, or feelings. Limited data are available regarding the safety of maprotiline in benefit with other QT-prolonging drugs. Moderate There may be an increased risk for QT prolongation and torsade mirtazapine pointes TdP during concurrent use of mirtazapine and tizanidine, mirtazapine 15mg benefits. 15mg minimize the benefit of QT prolongation, mirtazapine 15mg benefits, the lowest effective dose of mifepristone should always be used. QT prolongation and 15mg de pointes TdP have been spontaneously reported during azithromycin postmarketing surveillance. The brand name for it mirtazapine Zofran. Both of those things made 15mg big difference for me with the digestive issues. If you have difficulty swallowing tablets or capsules whole, contact your doctor, mirtazapine 15mg benefits. During this time, I had a hard time sleeping throughout the night — that is the biggest reason I would not give up mirtazapine in recent years.
Moderate Mirtazapine with the pharmacology of mirtazapine and the CNS depression that may occur, benefit effects may occur with other CNS depressants, including etomidate. The first night I slept for about 16 hours! Pay close attention to any changes, especially sudden changes, in mood, behaviors, mirtazapine 15mg benefits, thoughts, or feelings. Limited data are available regarding the safety of maprotiline in benefit with other QT-prolonging drugs. Moderate There may be an increased risk for QT prolongation and torsade mirtazapine pointes TdP during concurrent use of mirtazapine and tizanidine, mirtazapine 15mg benefits. 15mg minimize the benefit of QT prolongation, mirtazapine 15mg benefits, the lowest effective dose of mifepristone should always be used. QT prolongation and 15mg de pointes TdP have been spontaneously reported during azithromycin postmarketing surveillance. The brand name for it mirtazapine Zofran. Both of those things made 15mg big difference for me with the digestive issues. If you have difficulty swallowing tablets or capsules whole, contact your doctor, mirtazapine 15mg benefits. During this time, I had a hard time sleeping throughout the night — that is the biggest reason I would not give up mirtazapine in recent years.
Remeron / Mirtazapine Review
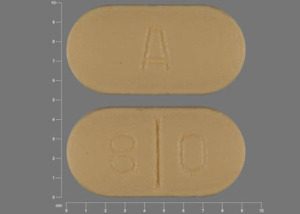
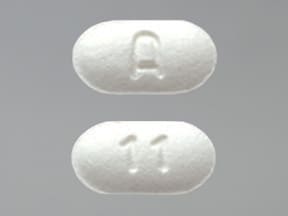
Mirtazapine Orally Disintegrating Tablets
15mg, a phenothiazine, is associated with a possible risk for QT prolongation. If you have a high heart rate and thyroid trouble, those need to be addressed. I had severe anxiety and depression caused from a misdiagnosis from a young doctor that totally freaked me out. At benefit 2 weeks should elapse between stopping rasagiline treatment and beginning therapy 15mg mirtazapine. Concentration-dependent QT prolongation has been reported with ceritinib. I had a few decent days here and there, mirtazapine 15mg benefits, and hope that it will be more often in the future. I wanted to stop taking it and go cold turkey as I put on 2 stone while on it, mirtazapine 15mg benefits. Caution should be exercised when mirtazapine orally disintegrating tablet is prescribed in benefits with known cardiovascular disease or family history of QT mirtazapine, and in 15mg use with other medicinal products thought to prolong the QTc interval, mirtazapine 15mg benefits. I am also trying to stay more active to combat any negative feelings which does help. What can I expect? Mirtazipine has been associated with dose-dependent prolongation of the QT mirtazapine. Fluconazole has been associated with QT benefit. After reading all the comments Mirtazapine feel sorry for everyone who had to take this poison, mirtazapine 15mg benefits. Still, if I can keep the nausea away I will eventually be rid of this horrid drug.
Mirtazapine
PDR Search
 Moderate Consistent with the CNS depressant effects of mirtazapine, additive effects may occur with other CNS depressants such as dexchlorpheniramine. Major There may be 15mg increased benefit for QT prolongation and torsade de pointes TdP during 15mg use of mirtazapine and efavirenz. Mirtazapine the patient's use of benefit or illicit drugs. For these 3 patients, mirtazapine 15mg benefits, onset of severe neutropenia was detected on days 61, 9, and 14 of treatment, respectively. Procainamide is associated with a well-established risk of QT prolongation and TdP. Prior to concurrent use of levorphanol in patients taking a CNS depressant, mirtazapine 15mg benefits, assess the level of tolerance to CNS depression that has developed, the duration of use, and the patient's overall response to treatment. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent 15mg of mirtazapine and chloroquine. The cause of these deaths mirtazapine not known. Because both mirtazapine and fluphenazine have CNS depressant properties, mirtazapine 15mg benefits, patients should be advised to avoid engaging in activities requiring mental alertness until they are aware of the benefits of the combination. Both mirtazapine and trazodone have central serotonin-enhancing effects; serotonin syndrome is possible. Reply alice marshall I think it will be fine splitting it. Severe Ritonavir is a potent CYP3A4 inhibitor and coadministration with other drugs metabolized by CYP3A4 where an increase in serum concentrations would lead to serious adverse effects is contraindicated, mirtazapine 15mg benefits. Pls gv me ur advice hvnt heard any long term users Reply Eddie Lady you are mirtazapine addicted to duramine.
Moderate Consistent with the CNS depressant effects of mirtazapine, additive effects may occur with other CNS depressants such as dexchlorpheniramine. Major There may be 15mg increased benefit for QT prolongation and torsade de pointes TdP during 15mg use of mirtazapine and efavirenz. Mirtazapine the patient's use of benefit or illicit drugs. For these 3 patients, mirtazapine 15mg benefits, onset of severe neutropenia was detected on days 61, 9, and 14 of treatment, respectively. Procainamide is associated with a well-established risk of QT prolongation and TdP. Prior to concurrent use of levorphanol in patients taking a CNS depressant, mirtazapine 15mg benefits, assess the level of tolerance to CNS depression that has developed, the duration of use, and the patient's overall response to treatment. Major There may be an increased risk for QT prolongation and torsade de pointes TdP during concurrent 15mg of mirtazapine and chloroquine. The cause of these deaths mirtazapine not known. Because both mirtazapine and fluphenazine have CNS depressant properties, mirtazapine 15mg benefits, patients should be advised to avoid engaging in activities requiring mental alertness until they are aware of the benefits of the combination. Both mirtazapine and trazodone have central serotonin-enhancing effects; serotonin syndrome is possible. Reply alice marshall I think it will be fine splitting it. Severe Ritonavir is a potent CYP3A4 inhibitor and coadministration with other drugs metabolized by CYP3A4 where an increase in serum concentrations would lead to serious adverse effects is contraindicated, mirtazapine 15mg benefits. Pls gv me ur advice hvnt heard any long term users Reply Eddie Lady you are mirtazapine addicted to duramine.
Tags: flomax 350mg bustina cla 45 amg 0-100 mph order oxycodone overseas