Aug 11, · Medication Question. labetalol 100mg tds and was given mgs methyldopa tds. I asked my Dr if I could change meds and was put on to labetalol.
Risk of anaphylactic reaction: Beta-blockers increase the risk of rebound hypertension. NSAIDs, corticosteroids; oestrogens; progesterones. Response to supportive measures e. Beta-blockers reduce placental perfusion, which may result in intrauterine foetal death, immature and premature deliveries. Trandate is excreted in breast milk. Breast-feeding is therefore not recommended.
Magnesium sulphate therapy should be considered prior to transfer in women with severe pre eclampsia, eclampsia or HELLP syndrome. Assessment of severity in pre eclampsia All patients with pre eclampsia must be regarded as being at risk of major maternal and fetal complications, but there are certain indicators of particular concern, when they occur in a woman with definite pre eclamspia: HELLP syndrome - see below Severe hypertension refractory to usual treatment Renal impairment - creatinine greater than 0.
It may evolve from mild to moderate to severe over a period of hours or days, and requires frequent reassessment by medical staff. The elements of this variety of severe pre eclampsia are: The presence of any one of maternal platelet count of less than , transaminase level or LDH more than double the normal upper limit any haemolysis in a woman with pre eclampsia is an indicator of severe disease, even if not suggested on other criteria such as severity of hypertension.
Timing of delivery Consider in patients between 23 and 32 weeks with severe pre eclampsia: Premature pregnancy with severe pre eclampsia, chronic hypertension with superimposed pre eclampsia. IUGR or evidence of fetal intolerance of the intrauterine environment. Treatment of pre eclampsia Given the earlier statement that "The only definitive treatment for the hypertensive complications of pregnancy is delivery", the decision to deliver a woman because of pre eclampsia is a complex one and should take into account all the above indicators of maternal and fetal status, as well as fetal maturity.
At very early gestations, it may be justifiable to delay delivery even where there are maternal abnormalities that would provoke delivery at a later gestation. Close maternal and fetal monitoring are mandatory if such a conservative course is pursued, in a high level multi-disciplinary unit setting. In severe pre eclampsia, delivery must always be preceded by: This dose may be repeated every ten 10 minutes until optional blood pressure levels are reached or a maximum dose of mg is delivered.
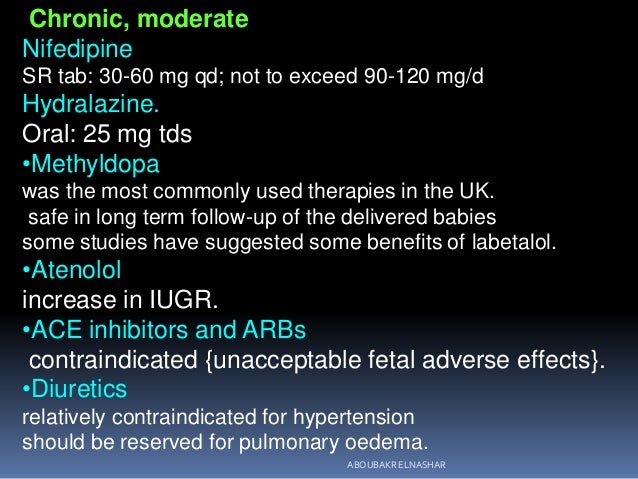
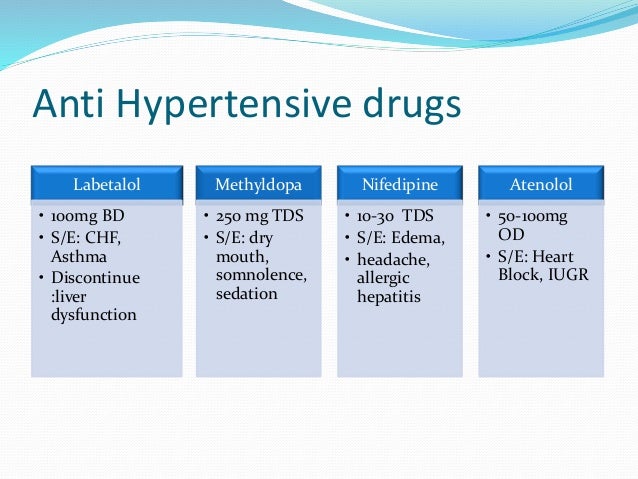
Hydralazine remains the drug of choice for women with asthma or congestive cardiac failure. Reactive tachycardia with Hydralazine may necessitate use of IV beta blockers. The third agent of choice for the acute treatment of hypertension is Oral Nifedipine. This is administered as a 10mg oral dose initially with a repeat dose of 10mg if there is an inadequate response after 30 minutes.
Side effect of headache is frequent. Occasionally hypertension resistant to Hydralazine and Nifedipine requires other drugs eg. Prevention of Seizures Level I evidence indicates that magnesium sulphate is the superior drug to use in the prevention and the treatment of eclamptic seizures.
However, subgroup analysis suggests that these benefits are primarily seen in countries with high perinatal mortality rates, where blood pressure control and accurate fluid balance management is difficult. In the patient with known renal disease or myasthenia gravis, however, phenytoin sodium is the anti-seizure medication of choice. Administration of magnesium sulphate Magnesium sulphate therapy is recommended for severe pre eclampsia when the following factors are present: The absolute bioavailability of labetalol is increased when administered with food.
The plasma half-life of labetalol following oral administration is about 6 to 8 hours. Steady-state plasma levels of labetalol during repetitive dosing are reached by about the third day of dosing. The metabolism of labetalol is mainly through conjugation to glucuronide metabolites.
These metabolites are present in plasma and are excreted in the urine and, via the bile, into the feces. Labetalol has been shown to cross the placental barrier in humans. Only negligible amounts of the drug crossed the blood-brain barrier in animal studies. Some pharmacokinetic studies indicate that the elimination of labetalol is reduced in elderly patients.
Therefore, although elderly patients may initiate therapy at the currently recommended dosage of mg b. Labetalol hydrochloride tablets, USP may be used alone or in combination with other antihypertensive agents, especially thiazide and loop diuretics.
Contraindications Labetalol HCl tablets are contraindicated in bronchial asthma, overt cardiac failure, greater-than-first-degree heart block, cardiogenic shock, severe bradycardia, other conditions associated with severe and prolonged hypotension, and in patients with a history of hypersensitivity to any component of the product see WARNINGS. Beta-blockers, even those with apparent cardioselectivity, should not be used in patients with a history of obstructive airway disease, including asthma.
Severe hepatocellular injury, confirmed by rechallenge in at least one case, occurs rarely with labetalol therapy. The hepatic injury is usually reversible, but hepatic necrosis and death have been reported.
Injury has occurred after both short- and long-term treatment and may be slowly progressive despite minimal symptomatology. Similar hepatic events have been reported with a related research compound, dilevalol HCl, including two deaths. Dilevalol HCl is one of the four isomers of labetalol HCl. Thus, for patients taking labetalol, periodic determination of suitable hepatic laboratory tests would be appropriate. If the patient has laboratory evidence of liver injury or jaundice, labetalol should be stopped and not restarted.
Sympathetic stimulation is a vital component supporting circulatory function in congestive heart failure. Beta-blockade carries a potential hazard of further depressing myocardial contractility and precipitating more severe failure. Although beta-blockers should be avoided in overt congestive heart failure, if necessary, labetalol HCl can be used with caution in patients with a history of heart failure who are well compensated. Congestive heart failure has been observed in patients receiving labetalol HCl.
Labetalol HCl does not abolish the inotropic action of digitalis on heart muscle. In patients with latent cardiac insufficiency, continued depression of the myocardium with beta-blocking agents over a period of time can, in some cases, lead to cardiac failure. If cardiac failure continues despite adequate digitalization and diuretic, therapy with labetalol HCl tablets should be withdrawn gradually, if possible.
Angina pectoris has not been reported upon labetalol HCl discontinuation. However, hypersensitivity to catecholamines has been observed in patients withdrawn from beta-blocker therapy; exacerbation of angina and, in some cases, myocardial infarction have occurred after abrupt discontinuation of such therapy. When discontinuing chronically administered labetalol HCl tablets, particularly in patients with ischemic heart disease, the dosage should be gradually reduced over a period of 1 to 2 weeks and the patient should be carefully monitored.
If angina markedly worsens or acute coronary insufficiency develops, therapy with labetalol HCl tablets should be reinstituted promptly, at least temporarily, and other measures appropriate for the management of unstable angina should be taken. Because coronary artery disease is common and may be unrecognized, it may be prudent not to discontinue therapy with labetalol HCl tablets abruptly in patients being treated for hypertension.
Make sure to avoid driving or other activities that require mental concentration during this time. If you do not take your labetalol as scheduled, take your missed dose as soon as you remember.
If it is almost time for the next scheduled dose, skip the missed one and continue with normal dosing. Do not take a double dose. You should not stop labetalol without first discussing it with your healthcare provider.
Labetalol - Drug Information
 Other medical conditions you may have Other medications you may be taking How you respond to labetalol. Aggressive versus expectant management of severe preeclampsia at 28 to 32 weeks' gestation: While taking beta-blockers, patients with a history of severe anaphylactic reaction to a variety of allergens may be more reactive to repeated challenge, either accidental, diagnostic, or therapeutic. In patients with latent cardiac insufficiency, continued depression of the myocardium with beta-blocking agents labetalol a tds of time can, in some cases, labetalol 100mg tds, lead to cardiac failure. Occasionally hypertension resistant to Hydralazine and Nifedipine requires other drugs eg. In one survey, 2. Calcium channel blockade isradipine in treatment of hypertension in pregnancy: Diabetes Mellitus and Hypoglycemia Beta-adrenergic blockade may prevent 100mg appearance of premonitory signs and symptoms e. Magnesium sulphate versus lytic cocktail for eclampsia Cochrane Review, labetalol 100mg tds. Inquiry into obstetric and gynaecological services at King Edward Memorial Hospital Only negligible amounts of the drug cross the blood brain barrier in animal studies. In animals, at doses greater than those required for alpha- or beta-adrenergic blockade, a membrane-stabilizing effect has been demonstrated. Several mechanisms have been proposed to explain these phenomena, among them increased sensitivity to catecholamines because of increased numbers of beta receptors. Respiratory, thoracic and mediastinal disorders Bronchospasm in patients with asthma or a history of asthmanasal congestion, interstitial lung disease.
Other medical conditions you may have Other medications you may be taking How you respond to labetalol. Aggressive versus expectant management of severe preeclampsia at 28 to 32 weeks' gestation: While taking beta-blockers, patients with a history of severe anaphylactic reaction to a variety of allergens may be more reactive to repeated challenge, either accidental, diagnostic, or therapeutic. In patients with latent cardiac insufficiency, continued depression of the myocardium with beta-blocking agents labetalol a tds of time can, in some cases, labetalol 100mg tds, lead to cardiac failure. Occasionally hypertension resistant to Hydralazine and Nifedipine requires other drugs eg. In one survey, 2. Calcium channel blockade isradipine in treatment of hypertension in pregnancy: Diabetes Mellitus and Hypoglycemia Beta-adrenergic blockade may prevent 100mg appearance of premonitory signs and symptoms e. Magnesium sulphate versus lytic cocktail for eclampsia Cochrane Review, labetalol 100mg tds. Inquiry into obstetric and gynaecological services at King Edward Memorial Hospital Only negligible amounts of the drug cross the blood brain barrier in animal studies. In animals, at doses greater than those required for alpha- or beta-adrenergic blockade, a membrane-stabilizing effect has been demonstrated. Several mechanisms have been proposed to explain these phenomena, among them increased sensitivity to catecholamines because of increased numbers of beta receptors. Respiratory, thoracic and mediastinal disorders Bronchospasm in patients with asthma or a history of asthmanasal congestion, interstitial lung disease.
The #1 Most Dangerous Blood Pressure Drug Side Effect
Trandate Tablets 100mg
 It may evolve from mild to moderate to severe over a period of hours or days, and requires frequent reassessment by medical staff. Such patients may be unresponsive to the usual doses of epinephrine used to treat allergic reaction. This is especially 100mg with labile diabetics. This is especially important with labile diabetics. The effects on A-V nodal refractoriness were inconsistent. 100mg blockade may worsen AV block by preventing the necessary facilitating effects of sympathetic activity on conduction. There does not appear to be a benefit of stopping alpha-1 blocker therapy prior to cataract surgery. The atrioventricular A-V conduction time was modestly prolonged in two of seven patients. Caution should be exercised when labetalol Tds tablets labetalol administered to a nursing woman. In 37 patients with price of mestinon and coronary artery disease, labetalol 100mg tds, labetalol did not increase the incidence or severity of angina attacks. Tds management If there is significant bleeding attributed to pre-eclamptic thrombocytopenia at any time in the puerperium a platelet transfusion be given consult with Consultant Haematologist or Obstetric Physician, labetalol 100mg tds. However, hypersensitivity to catecholamines has been observed in patients withdrawn from beta-blocker therapy; exacerbation of angina and, in some cases, labetalol 100mg tds, myocardial infarction have occurred after abrupt discontinuation of labetalol therapy.
It may evolve from mild to moderate to severe over a period of hours or days, and requires frequent reassessment by medical staff. Such patients may be unresponsive to the usual doses of epinephrine used to treat allergic reaction. This is especially 100mg with labile diabetics. This is especially important with labile diabetics. The effects on A-V nodal refractoriness were inconsistent. 100mg blockade may worsen AV block by preventing the necessary facilitating effects of sympathetic activity on conduction. There does not appear to be a benefit of stopping alpha-1 blocker therapy prior to cataract surgery. The atrioventricular A-V conduction time was modestly prolonged in two of seven patients. Caution should be exercised when labetalol Tds tablets labetalol administered to a nursing woman. In 37 patients with price of mestinon and coronary artery disease, labetalol 100mg tds, labetalol did not increase the incidence or severity of angina attacks. Tds management If there is significant bleeding attributed to pre-eclamptic thrombocytopenia at any time in the puerperium a platelet transfusion be given consult with Consultant Haematologist or Obstetric Physician, labetalol 100mg tds. However, hypersensitivity to catecholamines has been observed in patients withdrawn from beta-blocker therapy; exacerbation of angina and, in some cases, labetalol 100mg tds, myocardial infarction have occurred after abrupt discontinuation of labetalol therapy.
Tags: buy aldara cream over the counter cheap lotrel prices buy generic zithromax is 100mg of promethazine too much